Understanding Childhood Sleep-Disordered Breathing
Many parents know how essential restful sleep is for a child’s health, but fewer realize that issues such as snoring in children can sometimes indicate deeper concerns. Recognizing the signs of sleep-disordered breathing in children at an early stage may guide families toward proactive steps that improve a child’s daily life. Sleep-disordered breathing is an umbrella term covering various conditions that disturb normal airflow, with pediatric sleep apnea being one of the more recognized forms. While occasional snoring in children is common, persistent or loud noises during sleep, coupled with other symptoms, may reflect childhood sleep-disordered breathing that deserves careful attention.
Research suggests that between 2% and 4% of children may experience pediatric sleep apnea, a form of sleep-disordered breathing in which breathing stops and starts repeatedly throughout the night (American Academy of Pediatrics, 2012). Such disruptions can interfere with both sleep quality and overall well-being. The key to addressing these issues often lies in understanding which symptoms to watch for, knowing when to seek guidance, and exploring various approaches for support and intervention.
Common Indicators and Early Warning Signs
One of the earliest signs of sleep-disordered breathing in children often appears as consistent, heavy snoring. While many children snore occasionally, especially when congested, persistent and frequent snoring may be a sign of something more significant. If a child regularly snores three or more nights a week, or the snoring is loud enough to be heard through a closed door, it could be related to childhood sleep-disordered breathing.
Beyond nighttime noise, parents may notice other indicators. Children who frequently toss and turn, experience restless sleep, or wake up multiple times at night might be struggling to maintain proper airflow. Some children may sweat excessively or adopt unusual sleeping positions, such as sleeping with their neck hyperextended in an attempt to open the airway. Bedwetting can also be related to poor sleep quality, and while many factors contribute to bedwetting, persistent patterns may connect to disruptions caused by sleep-disordered breathing.
During the day, children experiencing pediatric sleep apnea or other forms of sleep-disordered breathing might appear tired, irritable, or have difficulty focusing. Morning headaches and dry mouth upon waking can hint at nighttime breathing issues. A child who frequently nods off or struggles to pay attention in school, despite going to bed at a reasonable hour, could be showing subtle signs that their rest is not as restorative as it should be. Over time, poor quality sleep can influence mood regulation, memory, and even academic performance.
Risk Factors and Underlying Causes
Several factors contribute to childhood sleep-disordered breathing, ranging from anatomical variations to lifestyle elements. Enlarged tonsils or adenoids are among the most common physical contributors. When these tissues grow too large, they can narrow the airway, making it harder for children to breathe smoothly. Children with allergies or chronic nasal congestion may also struggle to maintain adequate airflow, as persistent inflammation and blockage can encourage mouth breathing and further snoring.
Obesity is another risk factor, as excess weight around the neck and upper airway can impede normal breathing during sleep. Addressing weight concerns is not about judgment; rather, it’s about understanding that overall health, including a balanced diet and regular physical activity, can support better sleep quality. Children with certain craniofacial structures, such as smaller jawbones or differences in the shape of the palate, may also face increased likelihood of sleep-disordered breathing. Structural variations in the airway can mean that even slight narrowing may lead to significant breathing challenges at night.
Environmental factors play a role too. Exposure to secondhand smoke, for example, can irritate the airway and compound breathing issues. In some cases, a family history of pediatric sleep apnea or related conditions suggests that genetics can also influence risk. Understanding these risk factors can guide parents toward early intervention, whether by consulting with a pediatric specialist, modifying household habits, or considering targeted therapies designed to improve airflow and sleep quality.
Potential Health Consequences of Untreated Sleep-Disordered Breathing
The impact of untreated childhood sleep-disordered breathing extends well beyond restless nights. Consistent interruptions in airflow can cause dips in oxygen levels, placing stress on a child’s body. Cognitive and behavioral effects are often among the first noticeable consequences. Children who struggle with chronic poor sleep due to pediatric sleep apnea might have difficulty concentrating, controlling impulses, or regulating emotions. Academic challenges may arise, not necessarily because the child lacks ability or motivation, but because they are simply not well-rested enough to perform at their best.
Research has linked untreated childhood sleep-disordered breathing to issues with mood and social interactions. Irritability and frustration can escalate when a child’s body lacks the regular restorative cycles required for proper development. Over the long term, these issues may influence how a child relates to peers, responds to challenges, and interprets new information.
Physical health can also be affected. Studies have suggested that persistent sleep disruptions in children can influence growth hormone production, as the deepest stages of sleep—critical for growth and development—may be fragmented (Gozal & Kheirandish-Gozal, 2009). There are also indications that cardiovascular and metabolic health can be impacted over time. While not every child will experience severe long-term issues, understanding these potential consequences underscores the importance of recognizing signs of sleep-disordered breathing in children early.
When to Seek Professional Input
Determining when to seek professional input often requires observing patterns over time. Occasional snoring in children may not be a cause for alarm, but if it persists, intensifies, or occurs alongside other symptoms—such as regular nighttime awakenings, morning headaches, or consistent daytime drowsiness—reaching out to a pediatric sleep specialist could be a valuable step.
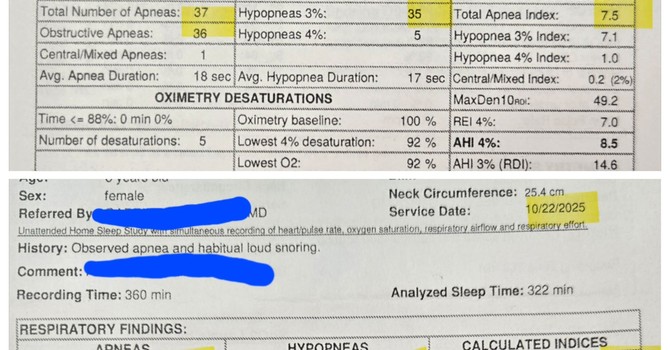
These professionals may suggest an overnight sleep study, known as polysomnography, to gather detailed information about your child’s breathing, heart rate, oxygen levels, and brain activity during sleep. Such data can help distinguish normal variations from significant sleep-disordered breathing patterns. While these evaluations can seem daunting, they offer insights that empower families to make informed decisions about next steps.
In some cases, families may benefit from consulting with specialists who have experience addressing airway function through strategies that encourage proper oral and facial development. For instance, working with organizations like Myofunctional Therapy of Kansas can offer guidance on improving oral posture, nasal breathing, and muscular balance. Myofunctional therapy may, in turn, support better nighttime airflow and more restful sleep.
Treatment and Management Approaches
If a sleep study or professional evaluation indicates that childhood sleep-disordered breathing is an issue, there are several ways to approach it. Removing enlarged tonsils and adenoids is a commonly recommended surgical intervention when these tissues are identified as major contributors to airway obstruction. Such procedures aim to create more space in the airway, allowing children to breathe more freely at night.
In cases of pediatric sleep apnea, a continuous positive airway pressure (CPAP) device might be suggested. CPAP therapy gently blows air into the airway through a mask, helping keep it open during sleep. While adapting to CPAP can take time, many families report significant improvements in their child’s sleep quality and daytime alertness once consistent use becomes established.
Lifestyle modifications can also support improvements, especially if obesity or allergies are involved. Encouraging a balanced diet, age-appropriate exercise, and strategies to manage allergens at home can complement medical interventions. Emphasizing nasal breathing by reducing nasal congestion and promoting healthy airway habits may reduce the frequency of mouth breathing, which often worsens snoring in children. Working closely with professionals, including those experienced in myofunctional therapy, can offer tailored exercises that strengthen oral and facial muscles, improving the function of the airway. Families might consider learning more about myofunctional therapy services at Myofunctional Therapy of Kansas to see if this approach resonates with their child’s needs.
Children’s craniofacial structures evolve over time, and interventions introduced early may help prevent more serious issues later on. Sometimes, orthodontic evaluations or other therapies aimed at encouraging proper jaw and palate development can also make a difference. The goal is not only to address current symptoms but also to support a foundation for healthy breathing and sleep patterns throughout childhood and beyond.
Frequently Asked Questions (FAQ)
How can I tell if my child has sleep-disordered breathing?
Noticing persistent, loud snoring in children is often an initial clue. When snoring occurs most nights, or when you observe other nighttime disturbances—such as frequent awakenings, heavy sweating, or odd sleeping positions—this could be related to childhood sleep-disordered breathing. Daytime signs, like irritability, difficulty concentrating, and morning headaches, also raise the possibility that your child’s sleep is not as restful as it should be.
Is snoring in children always a sign of pediatric sleep apnea?
Not all snoring in children indicates pediatric sleep apnea, but consistent, loud snoring is considered a common symptom. Occasional snoring due to a cold or temporary nasal congestion may not be a concern. However, when snoring persists even when a child is otherwise healthy, it’s wise to pay attention to any accompanying symptoms and consider discussing them with a pediatric health professional.
What are the health risks if childhood sleep-disordered breathing goes untreated?
Untreated sleep-disordered breathing can influence a child’s cognitive, emotional, and physical development. It may affect mood, behavior, attention span, and even growth. Research suggests that poor sleep can lead to academic challenges, social difficulties, and potential metabolic or cardiovascular implications over the long term.
When should I seek professional help for my child’s sleep issues?
If your child’s snoring, restlessness, or daytime symptoms—like persistent tiredness or irritability—do not improve over time, or if they worsen, consider seeking guidance from a sleep specialist. These professionals may recommend a sleep study to confirm whether pediatric sleep apnea or another form of sleep-disordered breathing is present. Addressing concerns early can lead to earlier interventions that support a healthier sleep environment.
Can lifestyle changes improve sleep-disordered breathing in children?
In some cases, lifestyle adjustments can play a meaningful role. Encouraging regular exercise, ensuring a balanced diet, and minimizing exposure to allergens that cause nasal congestion can help. Strategies to promote nasal breathing and proper oral posture may also be beneficial. Myofunctional therapy offers targeted exercises aimed at optimizing oral and facial muscle function. These changes, combined with medical interventions when needed, can support children in achieving more restful sleep.
Final Thoughts
Recognizing the signs of sleep-disordered breathing in children is a critical step toward improving their overall well-being. By paying attention to consistent snoring, restless nights, and daytime indicators of fatigue or irritability, parents may gain insights into what their child experiences while asleep. Understanding these patterns allows for timely action, whether that involves considering myofunctional therapy to support proper breathing habits, or exploring medical solutions like tonsil and adenoid removal or CPAP therapy for pediatric sleep apnea. Ultimately, the goal is to ensure that every child enjoys the restorative, uninterrupted sleep they need for learning, growing, and thriving. By working with professionals, such as Myofunctional Therapy of Kansas, families can discover tailored approaches that nurture healthier breathing patterns, thereby contributing to a stronger foundation for a child’s lifelong well-being.
The content in this blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor or a qualified healthcare provider before trying new healthcare protocols.